Soap Charting Ems
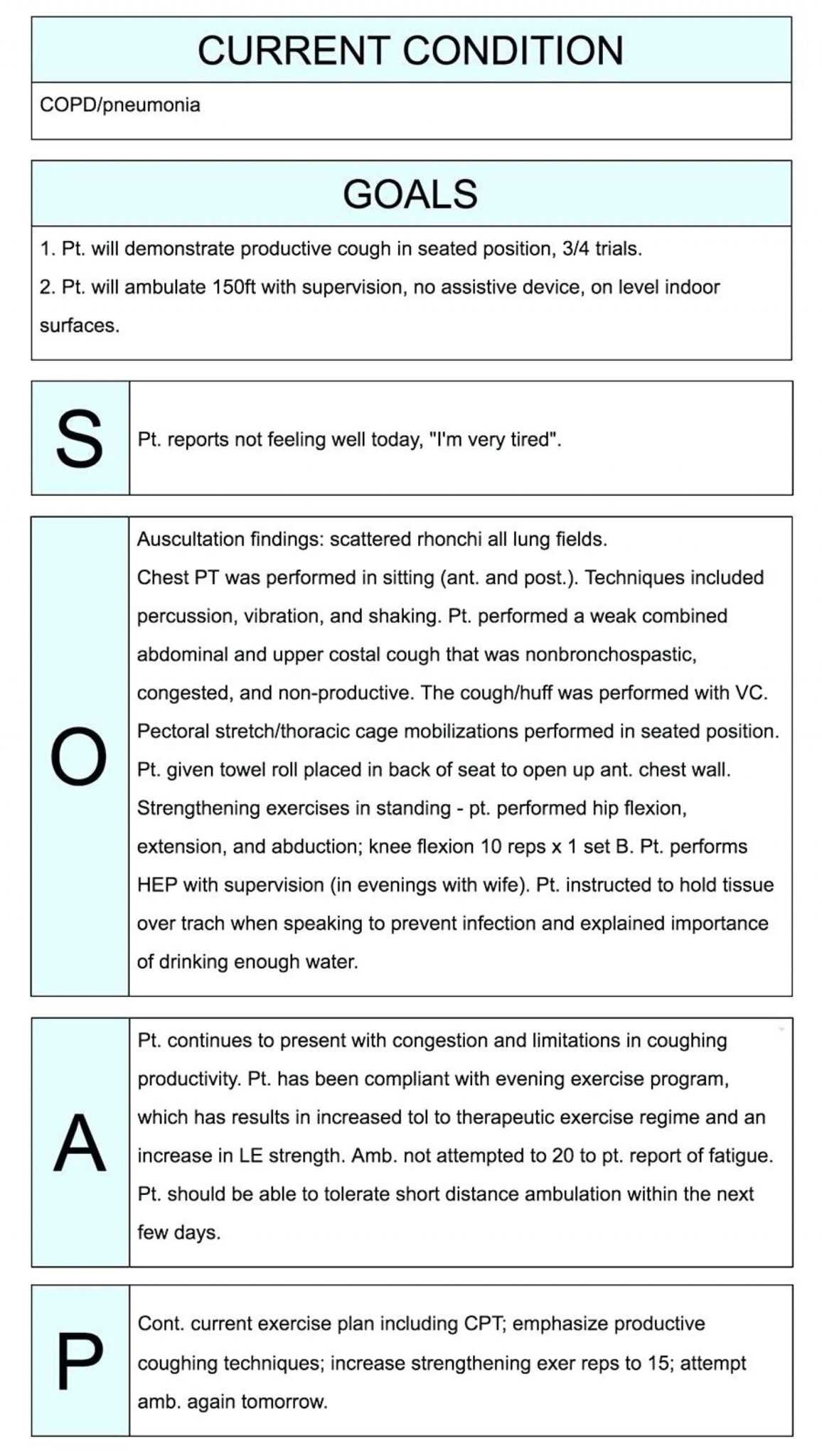
Soap Charting Ems - Visit online sunshine to access all florida statutes. Please contact mike hall, ems section administrator, at [email protected] for more information about ems rules and statutes. Web documenting a patient assessment in the notes is something all medical students need to practice. We will break down each component of a soap note and explain. Web today, the emergency medical services (ems) section is responsible for the licensure and oversight of over 60,000 emergency medical technicians and paramedics, 270+ advanced and basic life support agencies, and over 4,500 ems vehicles. Physical exam findings and level of consciousness. Web chances are you, like me, were told to paint a picture, tell a story, or to follow chart or soap mnemonics to ensure you capture details of a scene, creating effective, powerful stories in. What you were told by the facility, patient, and dispatch leading to you being sent to the call. Dispatched to a transport of a c/c going from to for unavailable at. In this area you will document anything that the patient or family & friends tell you. You do not need to format the narrative to look like this; Web today, the emergency medical services (ems) section is responsible for the licensure and oversight of over 60,000 emergency medical technicians and paramedics, 270+ advanced and basic life support agencies, and over 4,500 ems vehicles. Web soap (subjective, objective, assessment, and plan) is a mnemonic commonly used to. Physical exam findings and level of consciousness. Approximately 301 views in the last month. Please contact mike hall, ems section administrator, at [email protected] for more information about ems rules and statutes. Web ems rulemaking notices, workshops, and agendas. You can simply use these as an example of how to properly form a baseline structure for your narrative. This guides healthcare practitioners to systematically record subjective information, objective observations, assessments, and treatment plans, ensuring. Web soap is an acronym for a patient care report that includes: Physical exam findings and level of consciousness. Vital signs, including breath sounds. You do not need to format the narrative to look like this; Web chances are you, like me, were told to paint a picture, tell a story, or to follow chart or soap mnemonics to ensure you capture details of a scene, creating effective, powerful stories in. Web the soap note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by healthcare providers to write out notes. Web the chart and soap methods of documentation are examples of how to structure your narrative. Physical exam findings and level of consciousness. Web documenting a patient assessment in the notes is something all medical students need to practice. Web soap chart templates provide predefined sections for each component of the soap framework. The soap note is a way for. Web the soap note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by healthcare providers to write out notes in a patient's chart, along with other common formats, such as the admission note. The patient appears well nourished, well developed, and appears/does not appear to be in acute distress. Visit online sunshine to access. Web i have tried to use soap, chart, and any other way you can think of, but noticed i would tend to leave things out. The specific authority for the council, including membership and duties, is outlined in section. Find free downloadable examples you can use with healthcare clients. In this area you will document anything that the patient or. Web ems rulemaking notices, workshops, and agendas. Web the soap note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by healthcare providers to write out notes in a patient's chart, along with other common formats, such as the admission note. D// was dispatched out to above address in reference to for. Web i have. Physical exam findings and level of consciousness. Web learn how to write a soap note so you can efficiently track, assess, diagnose, and treat clients. Web chances are you, like me, were told to paint a picture, tell a story, or to follow chart or soap mnemonics to ensure you capture details of a scene, creating effective, powerful stories in.. D// was dispatched out to above address in reference to for. Physical exam findings and level of consciousness. Web the emergency medical services advisory council (emsac) was created for the purpose of acting as an advisory body to the emergency medical services (ems) section. The specific authority for the council, including membership and duties, is outlined in section. A soap. This guide discusses the soap framework (subjective, objective, assessment, plan), which should help you structure your documentation in a. Web ems rulemaking notices, workshops, and agendas. Web soap is an acronym for a patient care report that includes: Find free downloadable examples you can use with healthcare clients. Approximately 567 views in the last month. Web the soap note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by healthcare providers to write out notes in a patient's chart, along with other common formats, such as the admission note. Web the subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Web the chart and soap methods of documentation are examples of how to structure your narrative. You do not need to format the narrative to look like this; When the soap format is used, the chart is documented in the order of subjective complaints, objective findings, assessment notes,. A soap note is standard across all types of chart notes and can be used in any area of healthcare. Data that can be verified or observed by multiple people and get the same. Web chances are you, like me, were told to paint a picture, tell a story, or to follow chart or soap mnemonics to ensure you capture details of a scene, creating effective, powerful stories in. Web documenting a patient assessment in the notes is something all medical students need to practice. Chief complaint, moi or noi, sample including (pqrst), pertinent negatives. Please contact mike hall, ems section administrator, at [email protected] for more information about ems rules and statutes.
emt assessment cheat sheet Yahoo Image Search Results Emt study

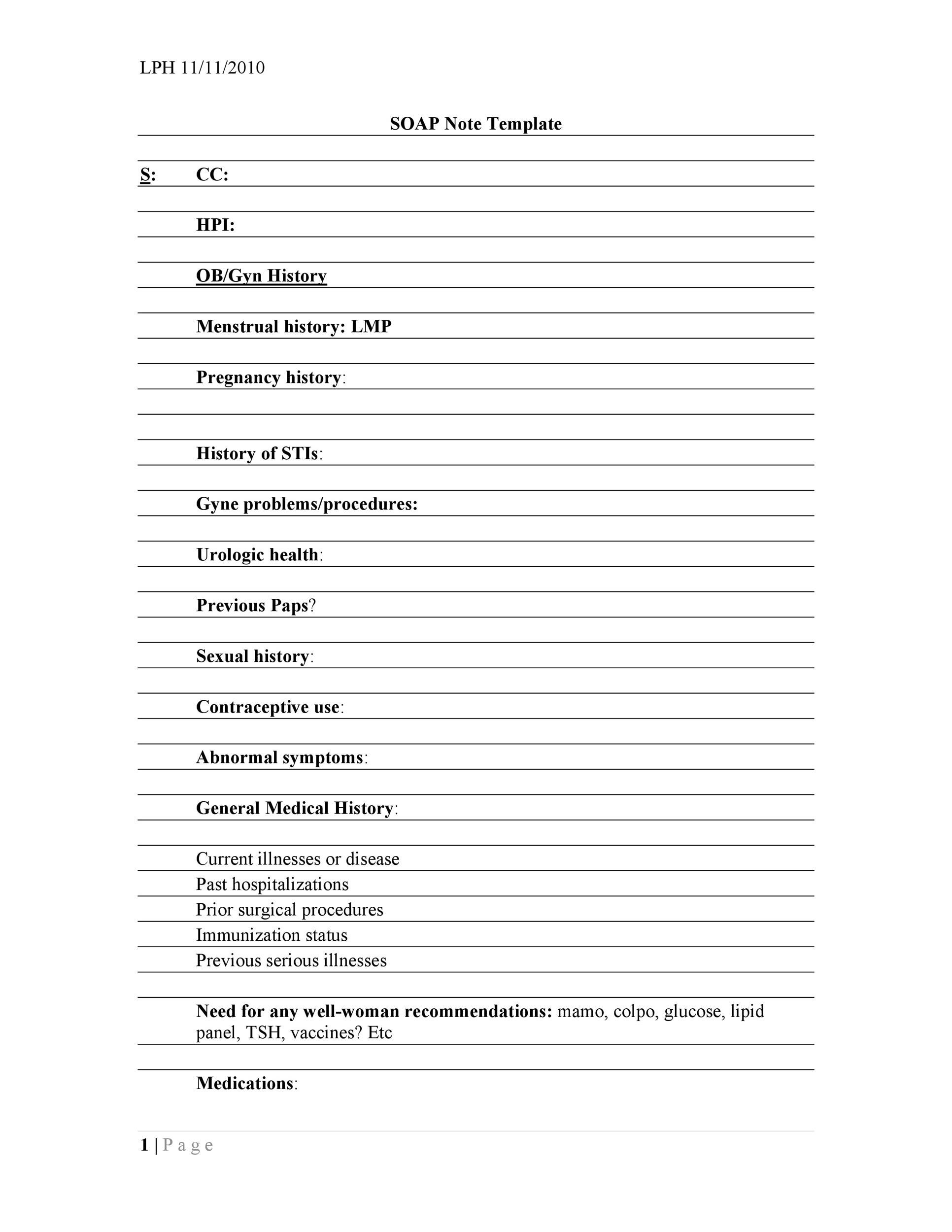
Soap Charting Template Ems

Soap Charting Template Ems
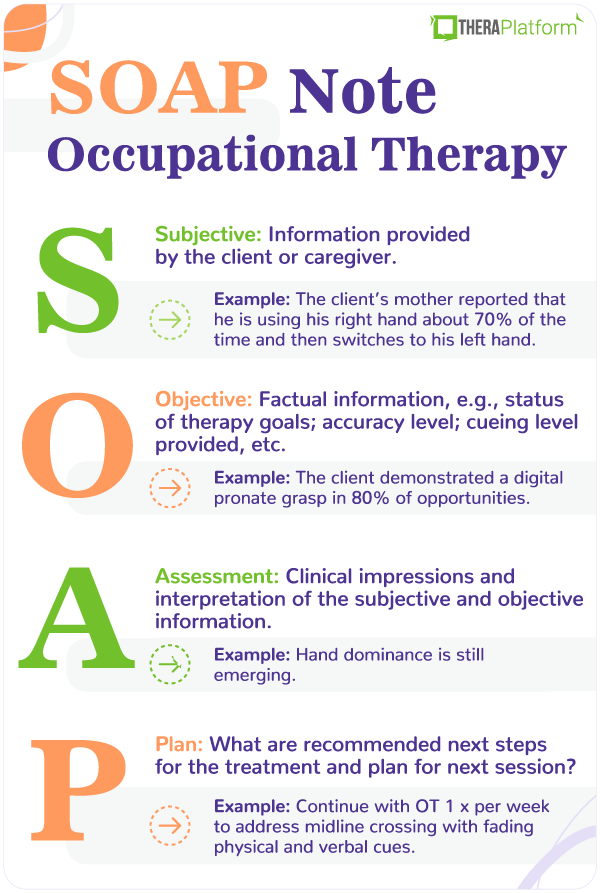
Occupational therapy SOAP note
Sample Soap Note Template
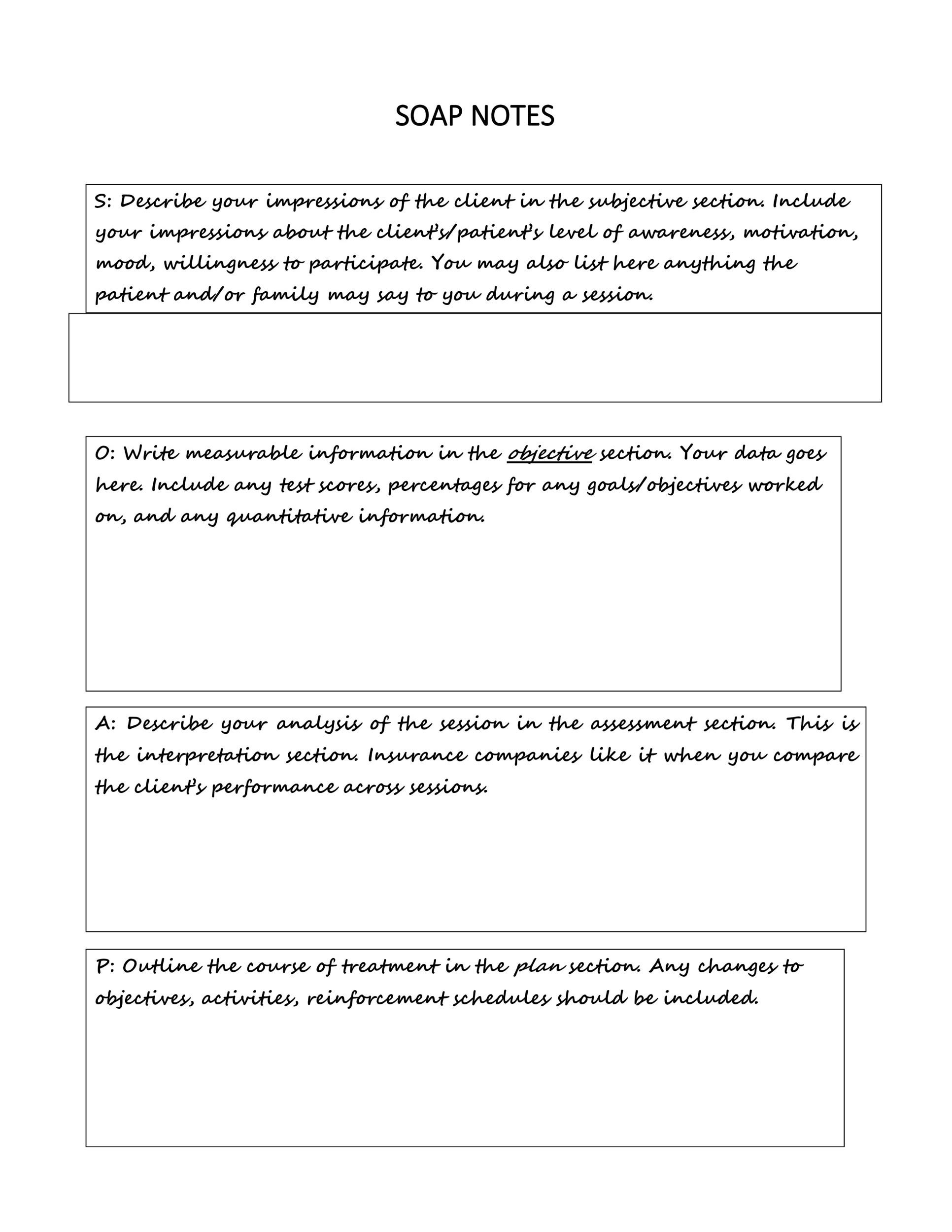
Soap Note Charting Examples

Pin by Vicky Kirkby on Nrsg notes Ems, Templates, Soap note
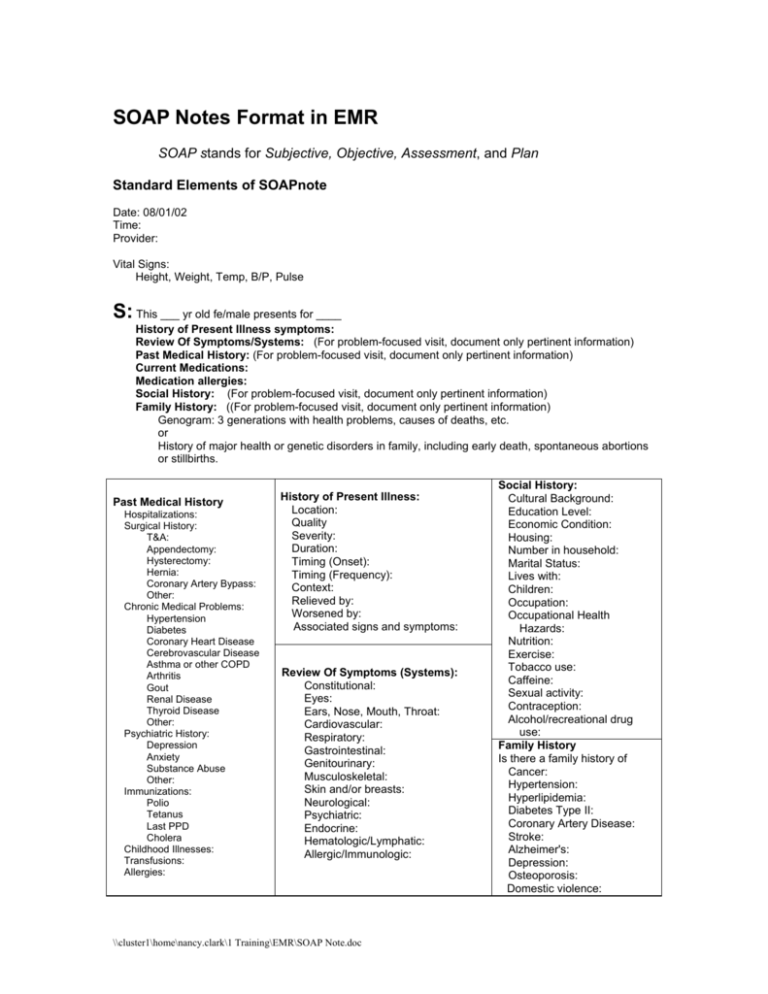
SOAP Notes Format in EMR
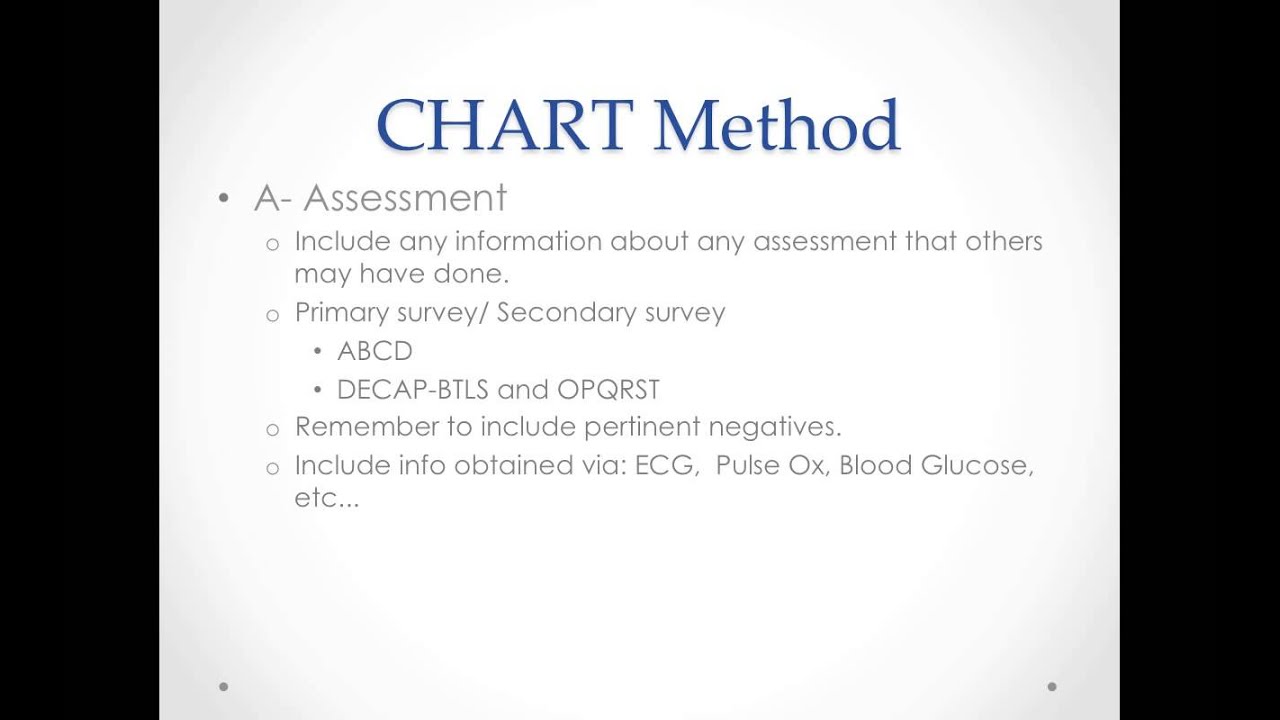
D Chart Method For Ems
023 Soap Note Example Mental Health Ems Format Template inside Soap
The Soap Note Is A Way For Healthcare Workers To Document In A Structured And Organized Way.
Visit Online Sunshine To Access All Florida Statutes.
The Patient Appears Well Nourished, Well Developed, And Appears/Does Not Appear To Be In Acute Distress.
(Abcds) And Secondary (Body Systems Head To Toe, So It's Easy To Remember).
Related Post: