Cvs Caremark Appeal Form Printable
Cvs Caremark Appeal Form Printable - To access other state specific forms, please click here. Once an appeal is received, the appeal and all supporting documentation are reviewed and completed, including a notification to the member and physician, within the following timelines: Web medicare coverage determination form. Who may make a request: Web appeal requests must be received within 180 days of receipt of the adverse determination letter. Your prescriber may ask us for an appeal on your behalf. Web our employees are trained regarding the appropriate way to handle members’ private health information. Full name of the person for whom the appeal is being filed. Web request for redetermination of medicare prescription drug denial. California members please use the california global pa form. California members please use the california global pa form. If you wish to request a medicare part determination (prior authorization or exception request), please see your plan’s website for the appropriate form and instructions on how to submit your request. Expedited appeal requests can be made by phone 24 hours a day, 7 days a week. Please complete one form. Web medicare coverage determination form. Because we, cvs caremark, denied your request for coverage of (or payment for) a prescription drug, you have the right to ask us for redetermination (appeal) of our decision. A clear statement that the communication is intended to appeal. If you wish to request a medicare part determination (prior authorization or exception request), please see. Web request for redetermination of medicare prescription drug denial. Please complete one form per medicare prescription drug you are requesting a coverage determination for. Full name of the person for whom the appeal is being filed. 711, 24 hours a day, 7 days a week. Once an appeal is received, the appeal and all supporting documentation are reviewed and completed,. A clear statement that the communication is intended to appeal. Once an appeal is received, the appeal and all supporting documentation are reviewed and completed, including a notification to the member and physician, within the following timelines: Full name of the person for whom the appeal is being filed. This form may also be sent to us by mail or. Web request for redetermination of medicare prescription drug denial. 711, 24 hours a day, 7 days a week. Who may make a request: Please complete one form per medicare prescription drug you are requesting a coverage determination for. This form may also be sent to us by mail or fax: Who may make a request: If you wish to request a medicare part determination (prior authorization or exception request), please see your plan’s website for the appropriate form and instructions on how to submit your request. To access other state specific forms, please click here. Web appeal requests must be received within 180 days of receipt of the adverse determination. Web appeal requests must be received within 180 days of receipt of the adverse determination letter. Full name of the person for whom the appeal is being filed. If you wish to request a medicare part determination (prior authorization or exception request), please see your plan’s website for the appropriate form and instructions on how to submit your request. To. Who may make a request: Web medicare coverage determination form. Your prescriber may ask us for a coverage determination on your behalf. This form may also be sent to us by mail or fax: Once an appeal is received, the appeal and all supporting documentation are reviewed and completed, including a notification to the member and physician, within the following. Please complete one form per medicare prescription drug you are requesting a coverage determination for. Full name of the person for whom the appeal is being filed. Your prescriber may ask us for a coverage determination on your behalf. If you wish to request a medicare part determination (prior authorization or exception request), please see your plan’s website for the. Your prescriber may ask us for a coverage determination on your behalf. This form may also be sent to us by mail or fax: Your prescriber may ask us for an appeal on your behalf. Web appeal requests must be received within 180 days of receipt of the adverse determination letter. Web our employees are trained regarding the appropriate way. Your prescriber may ask us for an appeal on your behalf. Full name of the person for whom the appeal is being filed. Your prescriber may ask us for a coverage determination on your behalf. Web request for redetermination of medicare prescription drug denial. Web medicare coverage determination form. Who may make a request: Once an appeal is received, the appeal and all supporting documentation are reviewed and completed, including a notification to the member and physician, within the following timelines: Expedited appeal requests can be made by phone 24 hours a day, 7 days a week. 711, 24 hours a day, 7 days a week. To access other state specific forms, please click here. Who may make a request: Web appeal requests must be received within 180 days of receipt of the adverse determination letter. If you wish to request a medicare part determination (prior authorization or exception request), please see your plan’s website for the appropriate form and instructions on how to submit your request. California members please use the california global pa form. Web our employees are trained regarding the appropriate way to handle members’ private health information. This form may also be sent to us by mail or fax: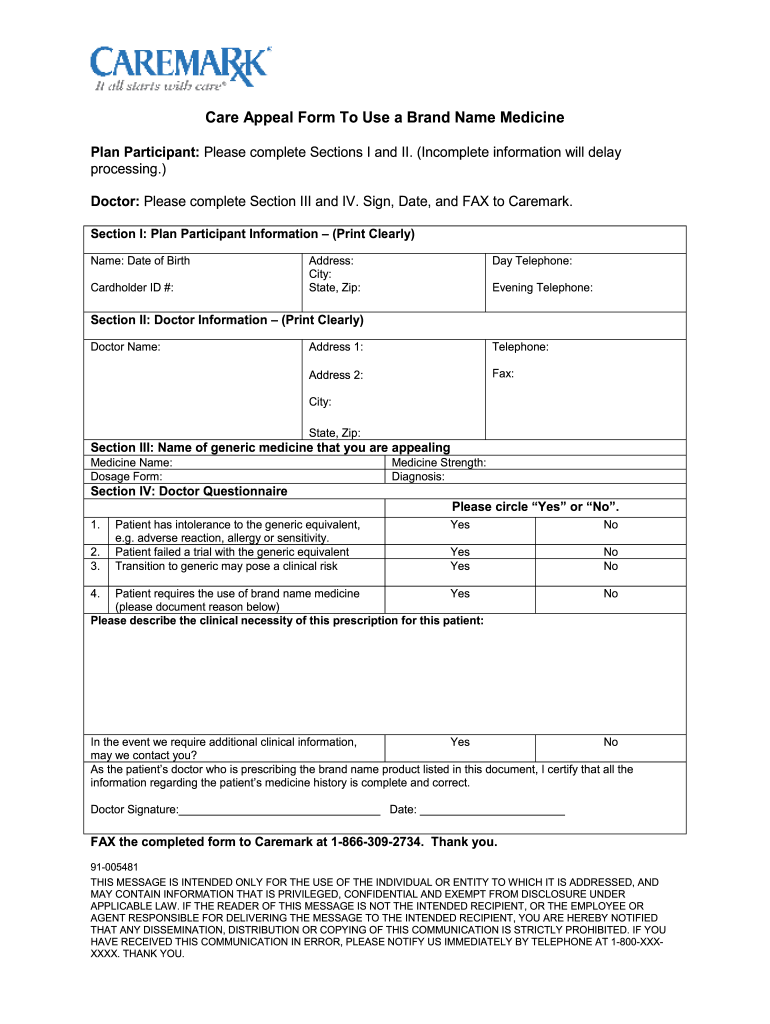
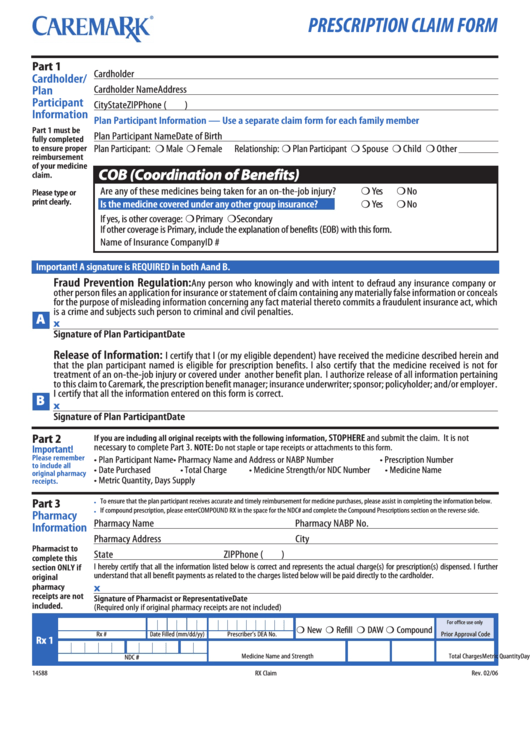
Cvs Caremark Appeal Form Edit & Share airSlate SignNow

Fillable Online Cvs Caremark Appeal Request Form. Cvs Caremark Appeal

Fillable Online Cvs caremark mac appeal form. Cvs caremark mac appeal
Top 20 Cvs Caremark Forms And Templates free to download in PDF format
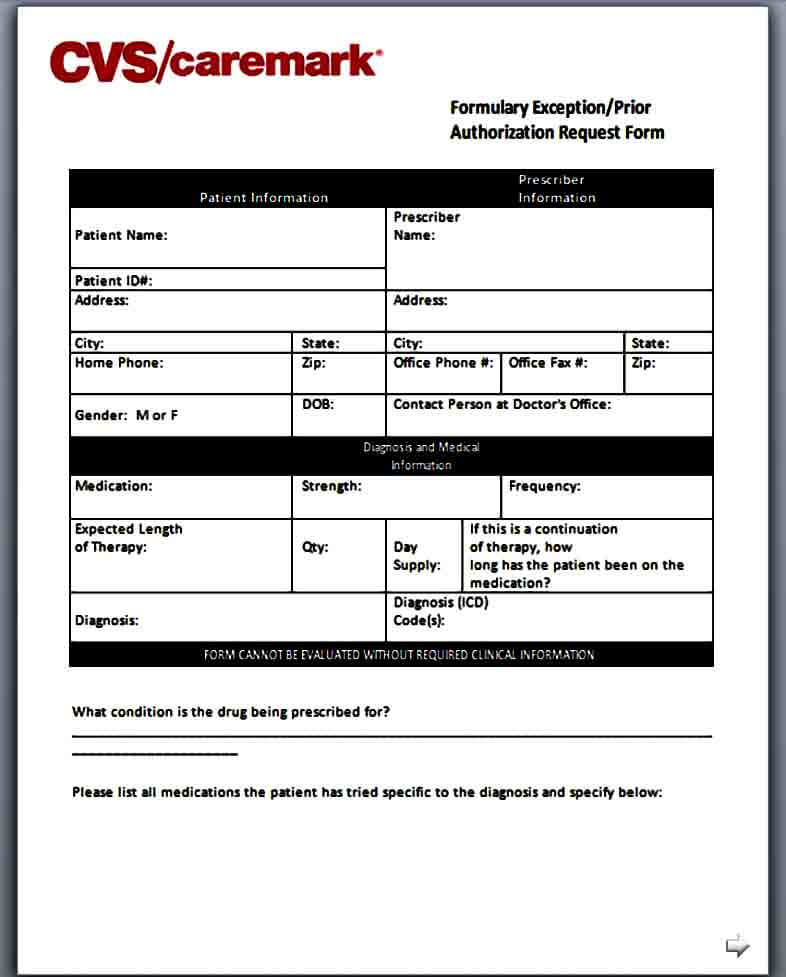
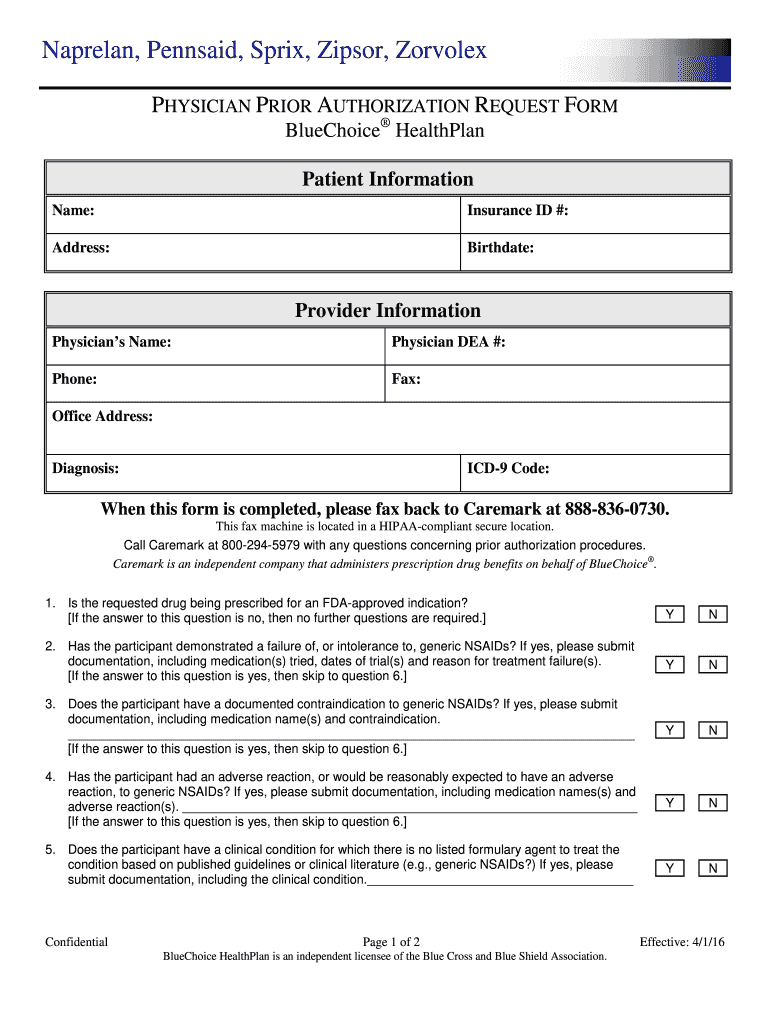
Template Caremark Prior Authorization Form Mous Syusa

Fillable Online bj proformancepcs Geha prescription appeal form cvs
Cvs Caremark Medicare Formulary 2024 Pdf Jane Jacklyn

Fillable Online Cvs caremark appeal forms. Cvs caremark appeal forms

Caremark Prior Authorization Request Form Fill and Sign Printable
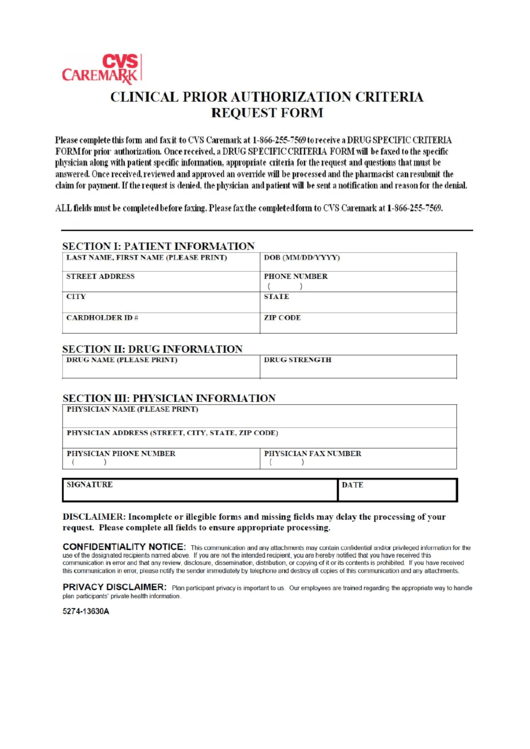
Caremark Prior Authorization Criteria Request Form printable pdf download
Please Complete One Form Per Medicare Prescription Drug You Are Requesting A Coverage Determination For.
Because We, Cvs Caremark, Denied Your Request For Coverage Of (Or Payment For) A Prescription Drug, You Have The Right To Ask Us For Redetermination (Appeal) Of Our Decision.
A Clear Statement That The Communication Is Intended To Appeal.
Web If A Form For The Specific Medication Cannot Be Found, Please Use The Global Prior Authorization Form.
Related Post: